Scientists Discover Small RNA That Regulates Bacterial Infection
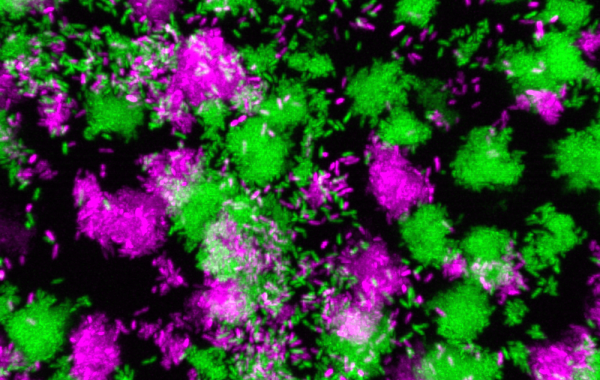
Pseudomonas aeruginosa clumps grown in synthetic cystic fibrosis sputum.
JUN 14, 2023 —
People with weakened immune systems are at constant risk of infection. Pseudomonas aeruginosa, a common environmental bacterium, can colonize different body parts, such as the lungs, leading to persistent, chronic infections that can last a lifetime – a common occurrence in people with cystic fibrosis.
But the bacteria can sometimes change their behavior and enter the bloodstream, causing chronic localized infections to become acute and potentially fatal. Despite decades of studying the transition in lab environments, how and why the switch happens in humans has remained unknown.
However, researchers at the Georgia Institute of Technology have identified the major mechanism behind the transition between chronic and acute P. aeruginosa infections. Marvin Whiteley – professor in the School of Biological Sciences and Bennie H. and Nelson D. Abell Chair in Molecular and Cellular Biology – and Pengbo Cao, a postdoctoral researcher in Whiteley’s lab, discovered a gene that drives the switch. By measuring bacterial gene expression in human tissue samples, the researchers identified a biomarker for the transition.
Their research findings, published in Nature, can inform the development of future treatments for life-threatening acute infections.
According to Whiteley and Cao, bacteria, like animals, are versatile and behave differently depending on their environment. A person with a chronic infection might be fine one day, but environmental changes in the body can cause bacteria to change their behavior. This can lead to acute infection, and a person could develop sepsis that requires immediate treatment.
“For years, people have been studying these bacteria in well-controlled lab environments, even though the lab is a place most microbes have never seen,” said Whiteley. “Our study took a novel approach to look directly into the bacterium’s behavior in the human host.”
The researchers chose to look at human tissue samples of chronic bacterial lung and wound infections. Using genetic sequencing technologies, Whiteley and Cao measured the levels of all types of mRNA present in the bacteria. The mRNAs encode the proteins that do all the work in a cell, so by measuring a bacterium’s mRNA level, one can infer the bacterium’s behavior.
While P. aeruginosa has roughly 6,000 genes, Whiteley and Cao found that one gene in particular – known as PA1414 – was more highly expressed in human tissue samples than all the other thousands of genes combined. The levels were so high that, at first, Cao and Whiteley thought the amount of PA1414 mRNA might be an artifact – a glitch associated with the sequencing methods.
“This particular gene is not expressed in the standard lab environment very much, so it was striking to see these levels,” Cao said. “And at this point, the function of the gene was unknown.”
The researchers also found that low oxygen drives the high expression of the gene. This is a common environmental characteristic of bacterial infections, as bacteria frequently encounter oxygen deprivation during chronic infections. Further tests showed that the gene also regulates bacterial respiration under low oxygen conditions.
Interestingly, the researchers found that rather than encoding a protein, the gene encodes a small RNA that plays a vital role in bacterial respiration. They named the small RNA SicX (sRNA inducer of chronic infection X).
The researchers then tested the functions of the gene in different animal infection models. They observed that when SicX wasn’t present, the bacteria easily disseminated from chronic infections throughout the body, causing systemic infection. The comparison allowed the researchers to determine that the gene is important for promoting chronic localized infection. Moreover, researchers also showed that the expression of SicX immediately decreased during the transition from chronic to acute infection, suggesting SicX potentially serves as a biomarker for the chronic-to-acute switch.
“In other words, without the small RNA, the bacteria become restless and go looking for oxygen, because they need to breathe like we need to breathe,” Whiteley said. “That need causes the bacteria to enter the bloodstream. Now, we know that oxygen levels are regulating this transition.”
Having a better indication for when an infection might enter the bloodstream would be a paradigm shift for treatments.
“If you can predict when an acute infection will occur, a patient could take a diagnostic test at home to determine if and when they may need to get treatment – before the infection becomes life-threatening,” Whiteley said.
The study provides answers to the long-standing questions about how and why chronic infections become acute. The researchers’ findings also open opportunities to develop therapeutics that target this specific molecular behavior associated with P. aeruginosa infections.
“The chronic Pseudomonas infection is usually highly resistant to first-line antibiotics,” Cao said. “By targeting this small RNA, we could potentially change the lifestyle of the bacteria to make it more susceptible to antibiotic treatments and achieve greater clearance of these dangerous infections.”
Citation: Cao, P., Fleming, D., Moustafa, D.A., et al. A Pseudomonas aeruginosa small RNA regulates chronic and acute infection. Nature 618, 358–364 (2023).

Marvin Whiteley

Pengbo Cao
